
Have you ever stuck your self with a needle or stepped on a fishing hook? Have you ever cut yourself so badly that it required stitches? Imagine having someone sewing up that cut with needle and thread but not using pain killer, not even aspirin or Tylenol. Have you ever had to dig a splinter out of your finger. Imagine having to dig a bullet or a 6 inch piece of wood out your side, again without any pain killers. Imagine is you can, the pain of having a leg or arm cut off without pain killers. Fortunately with today's healthcare, few people today have had limbs removed without the benefit of anesthetics or analgesics. Unfortunately many soldiers and some civilians are the targets of Improvised Explosive Devices and mines which are often designed to blow off arms so too many people know the pain of traumatic amputation. But imagine being told you will die if your leg is not cut off and you know that there is nothing that will kill the pain of the operation or recovery; that was the state of surgery in the Golden Age of Piracy.
Amputation
Amputations in the 18th Century were a risky business at best even when done by the most skillful surgeons. Until 1718, a leg amputation above the knee almost always ended in the the patient bleeding to death. In 1718, a French surgeon, Jean Louis Petit, invented the screw tourniquet this dramatically reduced deaths from bleeding to death and made it possible to successfully amputate a leg above the knee (thigh amputations). Unfortunately screw tourniquets did not stop the pain of the operation and if applied incorrectly caused mortification of the wound. The use of the screw tourniquet caught on relatively quickly among the learned surgeons but those in the outlying colonies or not schooled in a Surgeons College were less likely to know about the tourniquet or had the proper training to apply it correctly. By the time of the French and Indian War (1754) the use of the screw tourniquet was common practice among surgeons.
Blood loss was usually not the main cause of death from amputation, shock from the pain was most likely the leading cause of death from the actual amputation. Once again there was a disconnect between some common knowledge of the time and the conventional practice of the surgeon in the 18th century. Opium, a narcotic that lessens pain was well known in the 18th Century. Cocaine, another pain reducing drug was also known in the Caribbean However neither drug was seen as medicinally useful for another 100 years. The drug most commonly used to lessen pain was Strong spirits such as rum or whiskey. It was not effective for several reasons for more on pain killers see Analgesics and Anesthetics.
If the patient survived the injury that led to the need to remove a limb, survived the blood loss from the surgery and did not die from the intense pain of the operation, then he still needed to survive the almost certain infection that would follow the operation. Infection was not only common among amputees it was accepted as part of the healing process by many in the medical professionals of the time. The opinions on this progression of healing would slowly change so that by the 1770s only a very poorly taught surgeon would think infection was a necessary part of healing.
If an infection were to form, the laudable puss would show a few days after the operation. With the puss came high fevers and/or chills. After a few days of the laudable puss, fevers, and chills, if the patient responded well, the injury would start to heal and the patient would get well. If on the other hand, the patient did not start getting well, then further operations would follow or the patient would die. For more information on laudable puss see the entry on infection and mortification.
The actual procedure of amputating a limb was straight forward. Because of the lack of anesthetics speed was of the utmost importance. A good surgeon was able to remove an arm or leg in under ten minutes. In fact, even with the screw tourniquet it was necessary to remove the limb in less than 10 minutes to prevent the patient from dying from either shock or blood loss.
Up until the end of the 17th century most amputations were done with a straight cut through flesh and bone. By the end of the century and throughout the 18th century a two conical cut were made around the bone using a sharp surgeon's knife. this left the bone recessed inside the cone of flesh. In the case of remove a leg there were three major arteries that would be located and sutured closed. Afterwards a saw was employed to cut through the bone. Awash of water would follow the completion of the amputation in order to remove any bone fragments left on the exposed muscle and flesh. Once the leg or arm was removed, the cone was pushed together and sewn up to create a fleshy stub around the cut bone. Following the procedure bandages would be wrapped around the freshly amputated limb.
The major post operative problem with the surgery is sanitation was unknown and was not considered necessary. The bandage was not changed, the surgical knives and saws were not routinely cleaned, and it was not considered important to clean the wound area before or after the operation. In instances where a doctor may need to perform more than one surgery back to back, the blood of the first patient would quite often still be on the instruments when the doctor reached the second patient. The concept of spreading infection through bacteria or viruses did not exist because they had not been discovered yet. For more information on post operative infection see the entry on infection and mortification.

Amputation in the Operating Room of St. Thomas Hospital, 1775.
Visible on the left leg of the patient is a screw tourniquet.
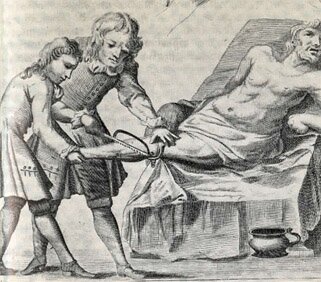
A 1716 engraving from the book Chirugea Curiosa>, by M.G. Purmann.
Two very different views of an 18th century leg amputation. The image to the left is closer to the actual scene, to the right the image as presented in a medical text of the time.
The Screw Tourniquet
Invented in 1718 by French surgeon Jean Louis Petit, the screw tourniquet made it possible to perform successful above the knee amputations. Because of the femoral artery which is fed by the abdominal aortic artery, blood loss in a thigh high amputation was almost if not always fatal. A regular strap tourniquet was not capable of stopping the flow of blood from the femoral artery. The screw tourniquet solved the problem.
The way the screw tourniquet worked is ingenious. The plate at the base of the screw is placed on the upper inner thigh above the femoral artery, midway between the cutting point and the groin. The loose ends are fed through the slot and cinched up tight on the hooks located on the top plate. Then the screw is turned, pulling the strap tight, until no pulse can be felt below the tourniquet. Once the blood flow from the femoral artery is cut the amputation could take place without the risk of blood loss. Of course shock and disease was still likely to claim the patient.
The application of the tourniquet had to be especially painful because it would also put enormous pressure on the sciatic nerve which runs down the lower back into thigh.
Analgesics & Anesthesia (pain killers)
The most common anesthetics used to date are derived from opium, cocaine, or for lesser pains forms of non-steroidal anti-inflammatory drugs-NSAIDs (aspirin, acetaminophen, ibuprofen). During the Golden Age, opium and cocaine existed but were not used medicinally. NSAID's were not even invented and only a few herbalists were aware of salicylic acid, a by-product of willow tree bark , a main ingredient in aspirin. In 1899 Bayer released his famous aspirin. Aspirin was actually invented by Wilhelm Siebel and Felix Hoffmann. They made acetylsalicylic acid which combines vinegar with salicylic acid to form a more useful product.
During the 18th century there was no aspirin but we do know that the medicinal usefulness of willow tree bark was known and had been known since ancient times. It was known by the ancient Greeks and remained common knowledge throughout Europe. It is also believed that the Native Americans knew of the its usefulness even before the arrival of the first Europeans. So while the professional doctors failed to recognize its usefulness to any great extent for some time to come, Quacks were most likely already selling patented creams that could cure acne, heal small abrasions, ease the pain of bruises and if taken by mouth calm a headaches. They would have made the cream from the bark of willow trees mixed with any kind of liquid that could soften the bark and allow it to be pulverized into a paste. The drug would have been somewhat effective yet just as quickly dismissed by the professional medical community.
Cocaine was used as a local anesthetic by the ancient Incans of Peru but its usefulness as a local anesthetic was not realized by Europeans until Carl Koller used it while performing eye surgery in 1884. It was used recreationally for much of the 19th century but was not well known during the Golden Age.
The more typical drug of choice for killing pain was a shot of rum or whiskey to help steady the nerves and to deaden the pain. In the popular literature, it was not uncommon for a surgeon to have a shot of whiskey with the patient before the operation. Alcohol made a poor analgesic at best. In order to be even remotely effective a patient would need to drink to the point of passing out which could easily be enough to cause alcohol poisoning or cause him to choke on his own vomit if he were to throw up while passed out. Even after drinking such an amount, it was still quite possible that the pain of the operation would wake him up. Thus typically, only a small drink would be given before the operation and possibly a little more after the limb was removed to help steady the nerves.
Probably the main deterrent to the use of pain killers was a lack of understanding of the nervous system. The study of the nerves or neurology did not fully come into existence until around 1681. And the connection between electricity and the nervous system was not understood until the end of the 18th century. Without this solid understanding of how the nervous system worked, it was difficult if not impossible for physicians and surgeons to develop a method for pain management. Most surgeons of the time considered shock the best anesthetic. They believed that the shock of the operation would shut down the patients nervous system and would prevent him from feeling the pain. What is more, they believed it was best to do the amputation quickly after the initial injury had occurred, believing the pain of the initial injury was enough to mask any future pain caused by the surgery, thus no type of pain management was really necessary. We know today they were wrong. Surgeons of the 18th century may have also known they were wrong but not having an effective pain remedy it becomes a moot point.
Bleeding

"Breathing a Vein", an 1804 engraving
by James Gillray
Bleeding was a common method for the treatment of several ailments, including infections from gun shot wounds, fevers, colds, gout, etc. Bleeding was only one of the more bizarre treatment methods. Other related treatments were purging, and cupping.
Bleeding was done in a number of way. One method was to apply leaches to the patient and let the leeches suck blood for a desired length of time. Another method involved the use of a lancet. The lancet was a spring loaded blade that would cut deep into a leg of forearm and open up a vein. The usual method was to apply a tourniquet around the leg or arm and then using the lancet, make an incision. Then the tourniquet would be loosened, the proper amount of blood would be allowed to flow into a measuring cup and then the bleeding would be stopped. as you can imagine, the lancet was not cleaned for antiseptic reasons but simply to keep it sharp and free from rust.
Purging is what it sounds like. A person would be fed something that would make him vomit or be given an enema to clean out his bowels.
Cupping involved placing a glass cup over a wound and then pressing down forcing the puss and blood to gush out of the wound. It would be similar to popping a black head except on a larger scale.
In some instances purging and cupping may have had some beneficial effects, however bleeding was rarely useful and this is why so much attention is paid on this harmful medical practice. As explained in the background section, bleeding was done in order to maintain a balance between the humors in body.
What is normally ignored when discussing bleeding during the 18th century is that there were physicians and surgeons who were questioning the logic of the procedure. Two such Doctors were Thomas Moffet and Cosimo Bonomo. By 1687 both men had determined that bleeding was useless when treating diseases or injuries. While main stream medicine disputed their findings, the men did have followers.
The Lancet
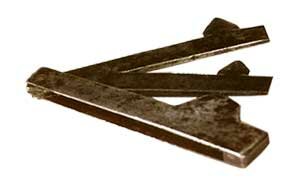
Pictured to the left is an 18th century lancet, a medical instrument used to open veins. It is debatable just how much pain was inflicted by the lancet but what is not debatable is the fact that virtually all pain inflicted by the lancet was misguided and unnecessary
The lancet was used by physician and surgeon alike.
Drowning
At the beginning of the 18th century people were not taught to swim and most people, even mariners did not know how to swim. Artificial resuscitation was at its infancy with many experts arguing over the merits of the practice. If a sailor fell overboard and the ship was moving at any great speed, it was often thought rescue was impossible unless he managed to grab a line or some type of floatation device could be thrown to him (an empty cask or something else that might float). Falling overobard was almost certain death and it was only the most stout hearted sailor who did not fear going overboard.
What was known is that people could be brought back from the dead, so to speak after being submerged in water for an extended time; even as long as thirty minutes. It was also known that a person who had been placed under the water for even a very short time minute could seemingly recover completely only to die a few hours or even a couple days later because of the submersion.
The pathogenesis or what is happening in the body while a person is drowning is quite complex and beyond the scope of this article to be discussed in detail. This is because the reaction of a drowning victim will vary according to the victim, the environment, and the situation.
The following factors are just a few of the details that will impact on the drowning episode was the person washed overboard in violent storm or did he fall overboard in still water while drunk? Depending on the situation, the body will react differently and different reactions will take place in the body.
- Did the person panic or did they remain calm
- Did the person have a chance to hold their breath or did they immediately swallow large amounts of water?
- In some instances of drowning the lungs may fill completely with water; in other cases very little water will be aspirated or breathed in.
- Drowning in salt water can bring about different reactions or long term consequences than a fresh water submersions.
The factors and others lead to hypoxia, acidosis, and finally cardiac arrest.
- Hypoxia
- A shortage of oxygen in the body, specifically in the blood stream
- Acidosis
- An increased acidity of the blood plasma
- Cardiac Arrest
- Heart failure (heart attack)
Most importantly for survivors of prolonged submersion is the linings of the lungs. The the lining of the lungs can be damaged during a submersion episode which can produce decreased lung capacity (an inability to take in oxygen) and if all the foreign fluid is not removed pneumonia can set in. In some instances of drowning, the stomach contents will be regurgitated and then breathed back into the lungs creating a new set of problems for the drowning victim.
So where does all this leave a drowning victim in the early 1700s? What kind of first aid was applied for a submersion victim 200 years before the concept of first aid existed? As mentioned, artificial resuscitation was in its infancy. Two methods were thought to be effective. One is very familiar to today’s lifeguards, mouth to mouth or mouth to nose resuscitation. The other method was to slip a tube of some sort down the trachea (breathing tube) and use a bellows to pump fresh air into the lungs (endotracheal tube).
Most trained doctors thought first method was inadequate because you were blowing used air into the lungs (and the stomach) and they discouraged its use while encouraging the trach tube and bellows. However, the second method involved a skilled physician who knew how to insert a tube into the trachea and also involved blowing air in with the bellows and then removing the bellows so the air could escape. In both cases, chest compression (that is, pressing on the external chest cavity in an attempt to start the heart) was not done. When you consider the tubes were not flexible and were not normally sanitized, you can see this method had many risks.
While bellows were carried on most ships where a fire was needed, they probably were not found on all ships or were not necessarily part of a sea surgeon’s medical chest, thus despite the thought that bellows were superior and tracheal tubes, most probably relied on mouth to mouth resuscitation.
The first step taken most people would have tried would have been to turn the person on their stomach and rub the back in an attempt to eject water from the lungs. Another method would be grabbing the person around the waist and repeatedly lifting the mid-section off the ground in an attempt to pump the water from the body. If the person seemed to be breathing after these attempts were made, a doctor would probably try to wake an unconscious victim by vigorous shaking. Despite the fact that mouth to mouth resuscitation was known before 1700, the above step would have probably been the only step taken by most sea faring men, especially pirates before 1700.
After 1700, if these first steps failed, then mouth to mouth or mouth to nose resuscitation would be performed. This involved a man placing his mouth over the drowning victim’s mouth or nose and then blowing air into the lungs. This would often involve two rescuers with one man blowing into the mouth while another man pushed down on the stomach to prevent the air from entering the stomach. Depending on the damage done to the linings of the lungs during the submersion, this type of resuscitation can be quite effective. In order for resuscitation to occur the alveoli must still be functional. The alveoli are the final branchings of the respiratory tree and act as the primary gas exchange units of the lung. The gas-blood barrier between the alveolar space and the pulmonary capillaries is extremely thin, allowing for rapid gas exchange. They are easily damaged when water is aspirated into the lungs.
If the alveoli is damaged severely enough, no amount of resuscitation will be successful. In other cases a person will be resuscitated but because of damage to the alveoli they will never regain lung capacity and in still other case the damage to the alveoli will progress over time and eventually kill the victim.
There was also rudimentary information regarding hypothermia or the loss of body heat, so the victim would probably be covered with blankets in an attempt to keep them warm so once a person appeared to be recovering they would probably be wrapped in blankets.
All sea going men knew that any time spent under the water could be deadly. Often for this reason, near drowning victims would be given rest or light duty for several days after the event even if they seemed alright.
Gunshot wounds
Despite what you see in the movies, in the 18th century a gunshot wound to the chest or abdomen was almost always fatal. That is to say if the bullet made it through the fat layer and entered into the actual chest cavity or intestines.
From Tobias Smollett's book we get this exchange:"the gentleman...asked what method of cure I would follow in wounds of the intestines. I repeated the method of care as it is prescribed by the best chirurgical writers, which he heard to an end, and then said with a supercilious smile, "So you think with such treatment the patient might recover?" I told him I saw nothing to make me think otherwise. "That may be," resumed he; "I won't answer for your foresight, but did you ever know a case of this kind succeed?" I acknowledged I did not, and was about to tell him I had never seen a wounded intestine; but he stopt me, by saying, with some precipitation, "Nor never will! I affirm that all wounds of the intestines, whether great or small, are mortal."
Unless the bullet could be seen or felt it was impossible to extract it. If the bullet had opened up the belly and exposed intestines, it was certain that peritonitis would follow. What was to follow was death. The only question was how long would death take and how much pain would the poor soul have to suffer. Surgery was not an option. About al the gun shot victim could do was pray and wait. On some occasions a bullet would lodge in the fatty tissue and work its way back out. In some cases no organ would be damaged and the person would go through life with a bullet lodged inside. however for most it was a slow lingering death from infection or internal bleeding.
Gun shots to the arm or leg could also prove fatal due to infection. Bullets had a nasty habit of pulling strands of filthy cloth into the body along with a note so sanitary bullet. most bullets were made of lead and often contained impurities. the act of firing the bullet from a pistol or musket did not as a common myth suggests, sanitize the bullet. They were dirty little balls of lead and would almost always lead to some kind of infection.
If the bullet hit a bone, amputation almost certainly followed. There was no way to set a bone that was shattered by a bullet, and the bone fragments were known to lead to infection. The only way to save the victims life was to take off the limb.
As for a gunshot that did not shatter a bone or injure organs, it was usually removed if the doctor could see it or feel it under the skin. Most doctors probed for bullets using their fingers. Once it was found they might use a bullet extractor or knife to cut out the bullet. Afterwards, the wound would be allowed to bleed in order to wash out any cloth and in hopes of preventing infection. Finally the wound would be sewn up, if necessary, and then bandaged.

A Surgeon's Bullet Extractor
The hollow tube has a spring loaded talon that grabs the bullet. The probe is inserted along the bullets path and if the bullet is found the handle is turned and hopefully the bullet is retrieved in one piece.
Quite worthless for deep abdominal or chest wounds.
Splinter wounds
Before you email me and tell me Myth Busters proved that splinter wounds didn't happen please read the following historically documented cases of splinter wounds:
Dead and wounded littered the deck, cut down by cutlass slashes, gunshots, and flying wood splinters gouged from the deck and rails by the hail of bullets. Loyall leaned exhausted against an aft cannon, himself bleeding from a splinter wound.
— (Historynet.com. American Civil War, the Bern Raid)
[Richard Dale] joined John Paul Jones's squadron as master's mate. Jones soon made him the first lieutenant of the Bonhomme Richard, and in that capacity he fought with distinction in the famous battle with the [HMS] Serapis, on 23 September 1779, and received a severe splinter wound (caused by large flying splinters of wood blasted out of the hull by enemy cannon shot).
— (Biographies in Naval History, Commodore Richard Dale)
During the battle, the air was thick with an infinity of savage wood splinters sent flying by the impact of the cannon balls shot through the wooden bulwarks. Projectiles of every kind imbedded themselves into human flesh; the slaughter was appalling. We have some details of the wounds suffered by the Shannons. The purser, George Aldham, grape shot in the lower part of the abdomen (lived one hour);... Private Dan Neil (Marine), splinter wound in the breast, several sabre wounds, bayonet wound in the belly -- the list of these men and their awful wounds goes on and on. Upwards to a 100 men on both sides who died on account of this twelve minute battle, all with the same sort of dreadful wounds.
— (History of Nova Scotia, Book #2: The Awakening. Part 5, The War Of 1812: Eastern Theatre. Ch. 12 - "The Shannon and the Chesapeake," Part 2.)
Bainbridge suffered two wounds during the fight. Early on a sniper's ball struck him in the hip; and, later, he sustained grievous splinter wounds when a cannonball shattered Constitution's wheel.
— (Dictionary of American Naval Fighting Ships, Bainbridge)
I could go on but I don't have the time or patience to look up the numerous cases of people wounded and killed by splinter wounds. There are literally hundreds of documented cases of people receiving grievous and even mortal wounds from wood splinters during a naval engagements. As much as like Myth Busters, the historical evidence proves that splinter wounds did happen and they were known to be lethal. I'm sure not every cannon ball that hit a deck caused splinter wounds. I'm just as sure lethal splinters were produced. Multiple cannon shots were bound to weaken the structure and causing splits in the wood. Follow up shots could then dislodged large splinters and greater speed than if the wood had maintaine dit's solid integrity. Myth Busters experimented a six pound cannon ball. They mentioned it would be ten times more lethal that the three pound ball. The long nines, were the chaser guns on many fighting ships firing a nine pound ball. Ships-of-war were often armed with 24 and 32 pounders. Pirate sloops often were armed with anything from 4 to 12 pounders. A salvo of 12 pounders followed up four minutes later by a second salvo could very well produce lethal splinters simply because the integrity of the ship's hull had been compromised . The historical evidence is proof that it did happen. The inability for two TV personalities to replicate a naval battle is not sufficient to debunk the factual record of splinter occurences.
While it is open to debate if more sailors and/or pirates were killed by splinter wounds than solid cannon shot, the splintering of the decks and sides of ships was well known and was considered one of the benefits of using solid shot against sailing ships. After repeated shots, the sides of sailing ships could be beat up bad enough that large splinters, well over a foot long, could be dislodged and become lethal wooden missiles. Smaller less deadly splinters could take out eyes or cause serious lacerations. If the splinter broke off in the process of pulling them form a body, infection would almost certainly follow. Often the only way to remove some splinters was by cutting them out. If the splinter went deep into the abdomen, the only way to safely remove it was by trying to pull it out. This was not always possible. Deep splinters to the vital organs were a slow and painful death. I'm sure the men who suffered such wounds wished they would have been a myth!
Infection & Mortification
It was important for both physician and surgeon to know the difference between infection and mortification. Infections could get better but mortified skin had to be removed. The most common way to remove mortified skin was through amputation when possible.
Today, we know that an infection is an invasion of a host by some foreign object. Typically this means inflammation caused by fungus, bacteria, or a virus but it can mean many other things. For instance, Colds are viral infections, athletes' foott is a fungal infection, and strep throat is a bacterial infection. Any numerous types of germs can cause wounds to become infected and in the 18th century almost all gun shot wounds would get infected to some degree. 18th Century doctors had no understanding of what caused infections. They did however know that wounds became infected. They referred to the discharge of an infection as laudable puss. Today, we know laudable puss as white blood cells in a wound fighting off an infection. In the 18th century this was considered a part of the healing process and in some ways it is. It is the body's attempt to fight off infection.
The puss was drained as part of the normal care of the wound. This was good in that they were also removing some of the infection but even draining the puss left it up to the body to fight off the infection. Laudable puss smelled foul but it did not smell like dead flesh. With luck the puss would eventually drain and the person would get better.
If the person did not get better, one of two things could happen. The infection could spread through the body via the circulatory system and the patient would die. Or the wound would mortify.
Mortification occurs when the wounded area no longer receives enough blood or air in order for the tissue to sustain itself. The most common term for mortification is gangrene. Gangrene (tissue death) is the rotting and decay of the flesh or body parts caused by infection or thrombosis or lack of blood flow. Typical sign of mortification is the stench of dead flesh, a blackening of the skin and painful swelling. The most common form of gangrene involving gun shot wounds or amputation was gas gangrene. Today we know it is caused by the clostridium perfringens bacteria. It spreads quickly and is still often fatal.

The only author and editor of all pages on the site. Most of what I write about is based on years of book reading on the topic. My first web page was published back in 1994.